Physical Therapy Treatment for Spastic Gait and Walking Rehabilitation
Spastic gait is one of the most common and complex walking impairments encountered in neurological rehabilitation. For physical therapists and rehabilitation centers, managing spastic movement patterns while promoting functional walking presents an ongoing clinical challenge. Increased muscle tone, impaired motor control, and reduced gait symmetry often limit a patient’s ability to practice safe, efficient ambulation.
What Is Muscle Spasticity From a Rehabilitation Perspective?
Muscle spasticity is a velocity-dependent increase in muscle tone caused by upper motor neuron dysfunction. From a functional standpoint, spasticity interferes with selective motor control, timing, and reciprocal muscle activation—key components of normal gait.
In the lower limbs, spasticity commonly manifests as:
- Reduced hip and knee flexion during swing
- Inadequate ankle dorsiflexion and foot clearance
- Stiff or circumducted gait patterns
- Asymmetry and increased energy expenditure
These impairments often contribute to
spastic gait or
spastic hemiparesis gait, particularly following stroke or other neurological injury.
Why Spastic Gait Requires Targeted Physical Therapy
Spastic gait is not solely a tone issue—it is a motor control and task-performance problem. Left unaddressed, it can lead to compensatory strategies, joint overload, and reduced community mobility.
Populations frequently presenting with spastic gait include:
- Individuals with spastic muscles after stroke
- Patients with traumatic brain or spinal cord injury
- People with progressive neurological conditions
For therapists and clinics, the primary goals are to:
- Improve gait efficiency and safety
- Increase walking repetition and task specificity
- Promote carryover beyond the clinic setting
Physical Therapy Treatment for Spastic Conditions Affecting Walking
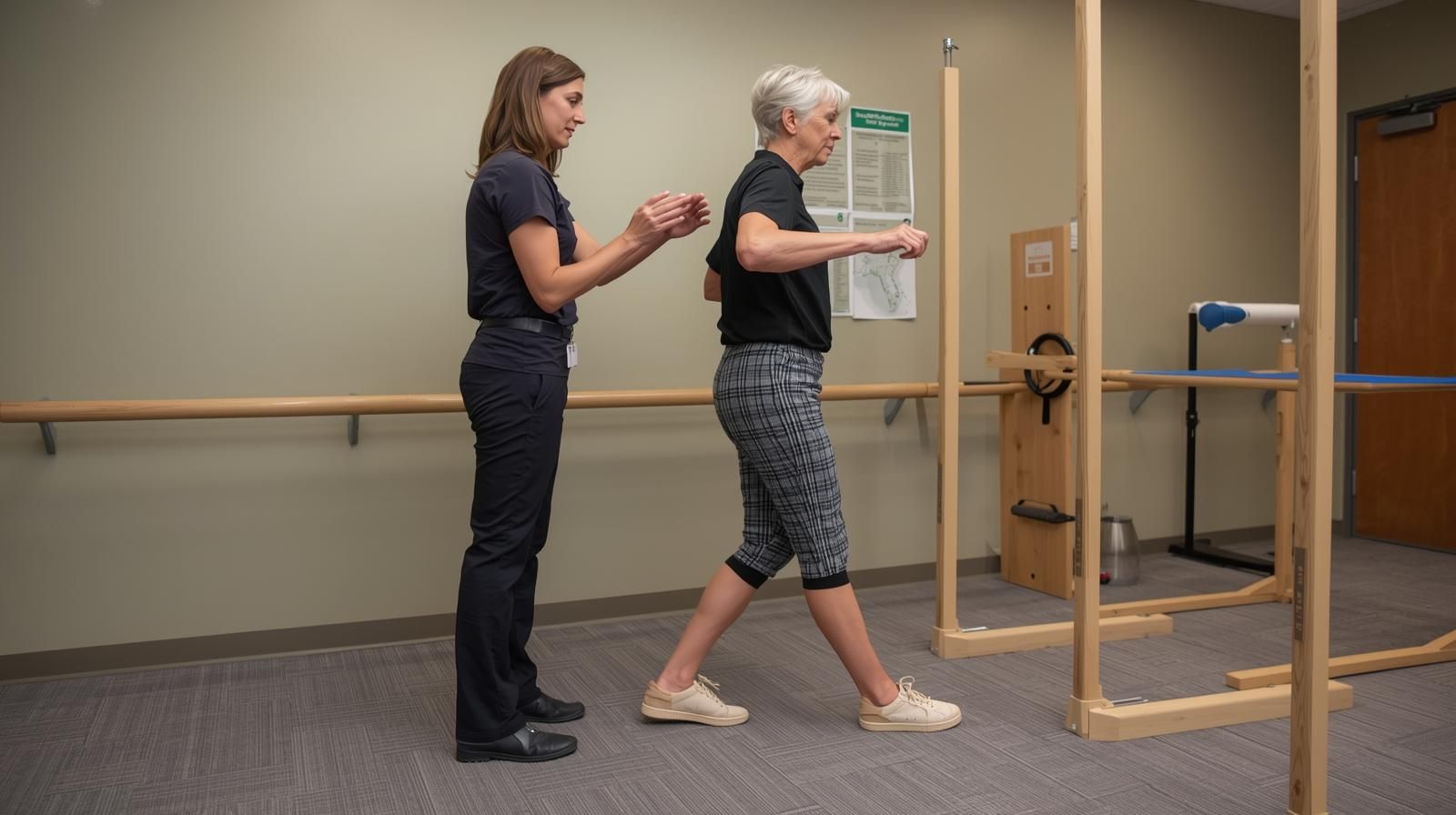
Task-Specific Gait Training
Repetitive, functional walking practice remains a cornerstone of neurorehabilitation. Task-specific gait training supports motor learning and neuroplastic adaptation, particularly when dosage and consistency are sufficient.
Leg Spasticity Exercises Integrated Into Function
Rather than isolated stretching alone, effective programs integrate leg spasticity exercises into functional movement patterns, emphasizing:
- Reciprocal activation
- Controlled swing-phase mechanics
- Progressive loading during stance
Spasticity Exercises and Motor Control
Spasticity exercises aim to reduce the functional impact of increased tone by improving movement sequencing, timing, and coordination—especially during transitional phases of gait.
Balance and Postural Control
Addressing postural stability is essential to reduce
fall risk and support independent ambulation, particularly in individuals with asymmetric gait patterns.
Supporting Gait Training Beyond the Treatment Session
Extending Therapy With Assistive Gait Devices
A common limitation in outpatient and inpatient rehabilitation is restricted walking dosage due to time, staffing, or patient fatigue. For physiotherapy centers, tools that enable safe, guided walking practice outside formal sessions can significantly enhance outcomes.
Clinical Role of Just Walk in Spastic Gait Rehabilitation
Just Walk by Chaban Medical is designed to support walking practice in individuals with neurological gait impairments. From a therapist’s perspective, it functions as a rehabilitation adjunct, not a replacement for therapy.
Clinically relevant benefits include:
- Assistance with leg lift during swing phase
- Encouragement of more symmetrical gait patterns
- Support for repetitive walking practice at home or in supervised settings
- Application across subacute and chronic neurological populations
For clinics, Just Walk can be integrated into:
- In-clinic gait training protocols
- Structured home exercise and walking programs
- Transitional care plans following discharge
👉 Product details: https://www.chaban-medical.com/just-walk-page
Clinical Considerations for Therapists and Centers
- Just Walk should be introduced following professional assessment
- Use is most effective when paired with clear gait goals
- Ideal for patients who can ambulate with supervision but need support for repetition and consistency
Positioning the device as a
therapy extender helps reinforce its role within evidence-based practice.
Summary
Spastic gait remains a multifactorial rehabilitation challenge requiring thoughtful clinical intervention. Physical therapy treatment for spastic conditions prioritizes task-specific walking, motor control, and repetition—elements essential for meaningful functional improvement.
For therapists and physiotherapy centers, combining skilled intervention with supportive walking tools can increase practice dosage, promote carryover, and enhance long-term mobility outcomes for patients with neurological gait impairments.
FAQ
?Does physical therapy reduce spasticity itself
Physical therapy primarily reduces the functional impact of spasticity by improving motor control and movement efficiency.
?Is walking practice recommended for patients with spastic gait
Yes, when appropriately assessed and supervised, walking practice is a key component of rehabilitation.
?Can assistive gait devices replace therapist-led treatment
No. Devices are best used as adjuncts to increase repetition and reinforce therapist-directed goals.
?Which patients are appropriate for gait-training support devices
Patients with neurological gait impairments who can ambulate with supervision and benefit from increased walking practice.
References
- American Physical Therapy Association (APTA) – Neurologic Physical Therapy Practice
- National Institute of Neurological Disorders and Stroke (NINDS) – Spasticity Overview
Important
This article is for informational purposes only and is not a substitute for professional medical advice; always consult your doctor or physical therapist before starting any exercise or using any device